Scottish COVID-19 inquiry Impact hearing| Health and social care|23 May 2024 (afternoon session)
NHS Glasgow porter of 25 years Neil Craig who speaks of ''half empty'' wards in 2020 during the peak of 'the pandemic'.
Introduction
Today’s session features NHS Glasgow porter and union representative for UNITE Neil Gray. Mr.Gray works within the Glasgow Royal Infirmary.
Extended highlights video featured below.
Testimony
‘‘At first as you remember it you and your colleagues were not getting COVID.’’
Reply- ‘Not at first.’ ——NO TEST=NO COVID.——??
‘‘They thought the workload was going to be higher…it turned out we we weren’t really needed.’’
‘‘Alot of patients were discharged out of the hospital either to home or care homes…the workload was definetely not as bad.’’
‘‘Your everyday general medicine patients…we were used to these wards being full to capacity most days
..but you’d go into those wards and they’d be half empty.’’
‘‘We had lots of free down time.’’
Even WITH ‘COVID’ patients wards still remained below normal capacity.
‘‘Gradually the workload would increase but still wouldn’t be anywhere near a normal day.’’
Statistics
As one can see compared to pre pandemic rates EMERGENCY depts in the Royal Infirmary were missing around 5,000 patients per month during the 2020 lockdown. Even by May the peak monthly admission rate was upto 4,500 patients up from 3,500 in March.
Total monthly admissions as follows:
April+May 2019=16,565
April+May 2020=8,067
A 50% decrease vs pre pandemic.
Below is planned operations (70% below normal) and emergency admissions (37% below normal) for the whole of NHS Glasgow 2020-2023.
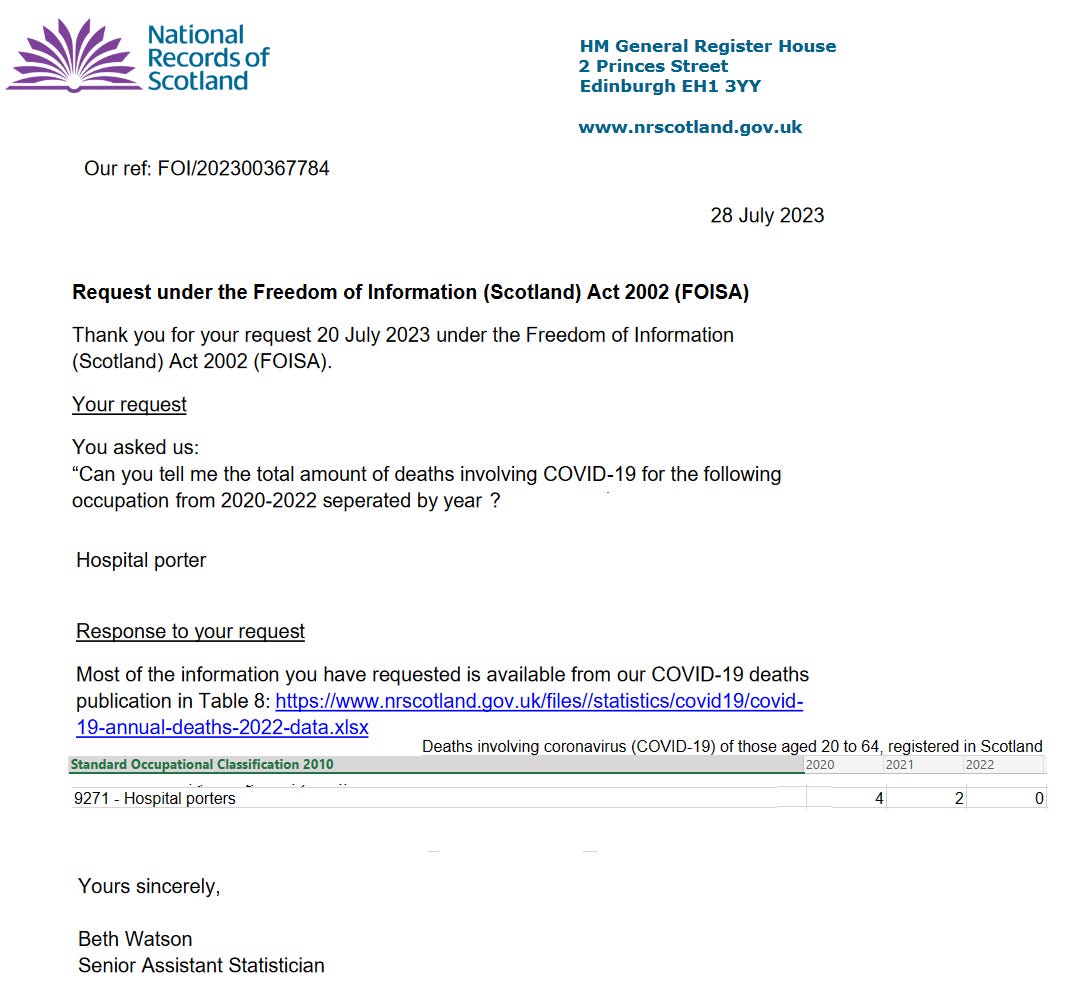
Deaths
According to National Records of Scotland 4 porters died in 2020 ‘involving’ COVID-19 2020-2022 from an employed workforce in the thousands.
Designated ‘‘COVID’’ wards
‘‘If one patient had COVID in a ward then that ward would become a COVID contact ward you couldn’t place patients in there.’’
‘‘Wards were changing sometimes you’d come in the morning but by the afternoon it was a COVID ward because someone tested positive.’’
‘‘You wouldn’t know you were going into a COVID ward at first unless you were told.’’
First ‘COVID case’ in a porter.
‘‘My first recollection of a porter with COVID was August 2020.’’
More staff sickness in 2023
Mr.Gray also mentions in his statement that staff sickness has been increasing from 2023.
Have experimental COVID-19 vaccines been a factor?
—A September 2023 study showed 35% of 1,704 enrolled healthcare workers had to call in sick after Covid 'vaccination' and sick leave significantly increased with each subsequent booster.
I could find no mainstream media reports of this testimony.
End
Links:
Full statement- https://www.covid19inquiry.scot/sites/default/files/ev-documents/sci-wt0118-000001.pdf
Full video-Scottish COVID-19 inquiry-Youtube-Impact hearing | Health and social care | 23 May 2024 (afternoon session)
https://www.sciencedirect.com/science/article/abs/pii/S0033350623002470










Its important to put 'Death in Service' into a context. Having worked in social care and the NHS for much of my career, I recall many cases of people of working age who died in service - and of course these are always a shock and upsetting.
e.g. In one hospital where I worked, we employed two porters who had learning difficulties - this was not unusual in the 1970's and 1980' - actually we even employed one head porter who was functionally illiterate - but very effective. One of the porters with a learning disability died of a strangulated hernia of some kind - very unexpected and sad. He was 35 or so.
Every year many tens of thousands of people of working age die in service - for all the usual reasons - mainly in my experience a brain haemorrhage or heart attack, or cancer - but suicides and road accidents are also not that unusual. I've lost colleagues to all of these, some very young indeed.
So, the new question is not how many NHS colleagues died OF covid, but how many WITH covid, and also, how different was this from a normal year's mortality in service?
Also, were deaths rates in the NHS in 2020/21 any different from the general population? As a former NHS Unison steward, these are the questions at the top of my mind, because obviously we all wish to see key staff protected as best as we can. If as I suspect the answer is 'no statistically significant difference' then we can rest assured that there was really no exceptional occupational risk.